Making a Difference for Those Impacted by Drug-Resistant Tuberculosis
By: Abhijit Barve
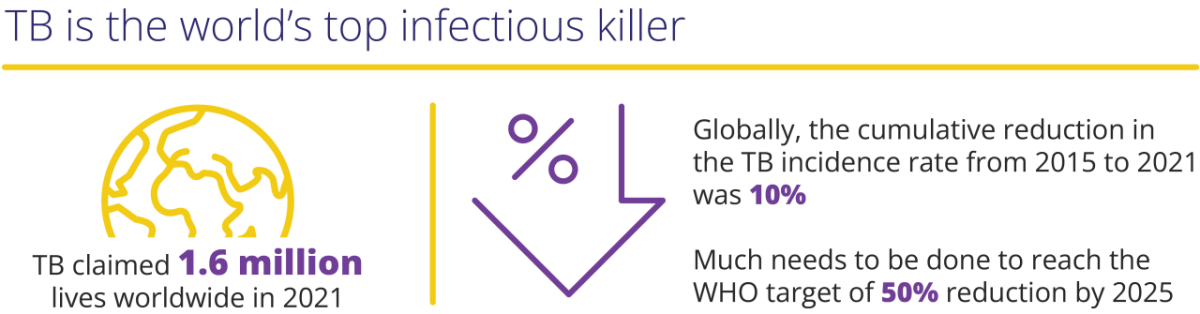
Tuberculosis (TB) remains one of the world’s deadliest infectious diseases, second only to COVID-19, claiming 1.6 million lives worldwide in 2021.1 TB generally affects the most vulnerable people – those who live in poverty, are marginalized or economically and socially excluded.2 Ongoing conflicts across Eastern Europe, Africa and the Middle East have further exacerbated this situation.3 Globally, the cumulative reduction in the tuberculosis incidence rate from 2015 to 2021 was 10% and has faced significant setbacks due to COVID-19 disruptions in care.4 Much more needs to be done to reach the World Health Organization’s (WHO) End TB Strategy milestone target of 50% reduction by 2025.5
Multi-Drug Resistant TB (MDR-TB) remains a growing public health crisis, with only about one in three people accessing treatment in 2020.1 Multi-Drug Resistant/Rifampicin-Resistant (MDR/RR) and Extensively Drug-Resistant (XDR) TB, together commonly referred to as DR TB, represent the greatest threat to the progress that has been made, especially as COVID-19 disruptions negatively impacted treatment.
The significance of DR TB within the broader context of Antimicrobial Resistance
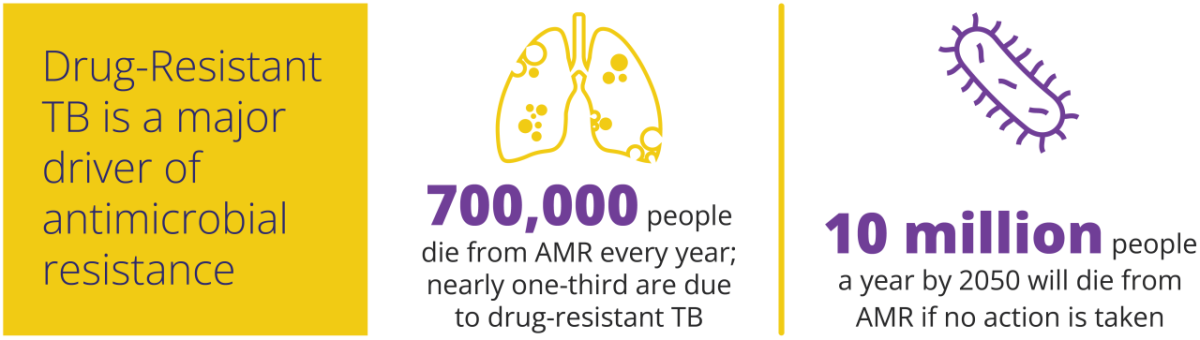
Drug-resistant TB is a major driver of antimicrobial resistance (AMR).6 Of the 700,000 people the WHO estimates die every year from AMR, nearly one-third are due to drug-resistant TB – by far the largest single contributing cause. The WHO estimates that the number of deaths due to AMR could rise to 10 million people a year by 2050 under the most alarming scenario if no action is taken.7
Increasing Global Access to Treatment
Providing sustainable access to high-quality medicines and healthcare is a universal need. At Viatris, we realized that we had a powerful platform, as the world’s largest producer of HIV drugs by volume, to help those living with TB around the world, including the regions where the TB burden is the highest – in low- and lower- middle-income countries. As such, our commitment to access begins with our ability to sustainably deliver high-quality medicines to people, regardless of geography or circumstance, and we offer a range of anti-TB medication options. Our efforts extend beyond delivering treatment options, as we believe that increased awareness and education are also crucial to help advance the WHO’s treatment recommendations, which include MDR-TB guidance.
These steps to expand access to healthcare for previously unmet needs of patients suffering from DR-TB are a small part of the global fight to end TB. We know we can do more – and are committed to continue partnering to make a difference for those impacted by TB.
India:
TB remains a pressing public health concern in India – the country shoulders a significant portion of the global TB burden. Viatris has partnered with the Government of India and non-governmental and civil society organizations for many years to improve TB care in India. In a dedicated effort to combat the disease and improve treatment outcomes, HEAL Foundation, supported by Viatris, recently launched the India Fights TB initiative. The new program aims to spread awareness and enhance treatment adherence among TB patients in India. Partnerships and collaborations such as these are critical to support early diagnosis and enhance treatment adherence.
Other key initiatives in India have included:
- Partnered with India’s planning commission to increase awareness, enhance screening and provide access to quality healthcare in the model district of Bahraich in Uttar Pradesh
- Facilitated screening of over 1 million people and helped 700 patients access the public health TB program
- Recognized by United States Agency for International Development (USAID) for contributions to expanding access to TB health in India under the TB Pledge formulated in 2019
South Korea:
With the highest rate of TB incidence among OECD (Organisation for Economic Co-operation and Development) members*, TB remains a serious public health problem in South Korea. Viatris has worked to develop critical partnerships and collaborations to support sustainable access to medicines for TB patients in South Korea. Together with an array of organizations including medical thought leaders, the Ministry of Health and Welfare, the Korea Centers for Disease Control and Prevention, and the STOP TB international network, access for a new XDR-TB treatment was achieved, making it possible to facilitate care for XDR-TB patients without a charge or delay.
*Source: https://www.who.int/teams/global-tuberculosis-programme/tb-reports
References:
1 World Health Organization. Tuberculosis. [Internet]. 2023 [cited 2023 Aug 17]. https://www.who.int/news-room/fact-sheets/detail/tuberculosis
2 Equi-TB. [Internet]. 2022 [cited 2023 Aug 17]. https://assets.publishing.service.gov.uk/media/57a08c98e5274a31e00012fa/HTBLivtb_vulnerable.pdf
3 World Health Organization. Tuberculosis deaths and disease increase during the COVID-19 pandemic. [Internet]. 2022 [cited 2023 Aug 17]. https://www.who.int/news/item/27-10-2022-tuberculosis-deaths-and-disease-increase-during-the-covid-19-pandemic
4 World Health Organization. Global tuberculosis report 2022. Geneva: World Health Organization; 2022. License: CC BY-NC-SA 3.0 IGO.
5 World Health Organization. The End Tb Strategy. [Internet]. 2015 [cited 2023 Aug 17]. https://www.who.int/publications/i/item/WHO-HTM-TB-2015.19
6 World Health Organization. The End Tb Strategy. [Internet]. 2015 [cited 2023 Aug 17]. https://www.who.int/activities/tackling-the-drug-resistant-tb-crisis
7 O’Neill J. Tackling drug-resistant infections globally: final report and recommendations. Review on Antimicrobial Resistance. 2016. [accessed April 15, 2017] https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf